Outlive: The Science and Art of Longevity (Peter Attia)
A groundbreaking manifesto on living better and longer that challenges the conventional medical thinking on aging and reveals a new approach to preventing chronic disease and extending long-term health, from a visionary physician and leading longevity expert.
Wouldn’t you like to live longer? And better? In this operating manual for longevity, Dr. Peter Attia draws on the latest science to deliver innovative nutritional interventions, techniques for optimizing exercise and sleep, and tools for addressing emotional and mental health.
These are my reading notes from this book. All errors, omissions, and misrepresentations are mine.
- Chapter 1: The Long Game – From Fast Death to Slow Death
- Chapter 2: Medicine 3.0 – Rethinking Medicine for the Age of Chronic Disease
- Chapter 3: Objective, Strategy, Tactics – A Road Map for Reading This Book
- Chapter 4: Centenarians – The Older You Get, the Healthier You Have Been
- Chapter 5: Eat Less, Live Longer? – The Science of Hunger and Health
- Chapter 6: The Crisis of Abundance – Can Our Ancient Genes Cope with Our Modern Diet?
- Chapter 7: The Ticker – Confronting—and Preventing—Heart Disease, the Deadliest Killer on the Planet
- Chapter 8: The Runaway Cell – New Ways to Address the Killer that is Cancer
- Chapter 9: Chasing Memory – Understanding Alzheimer’s Disease and Other Neurodegenerative Diseases
- Chapter 10: Thinking Tactically – Building a Framework of Principles that Work for You
- Chapter 11: Exercise – The Most Powerful Longevity Drug
- Chapter 12: Training 101 – How to Prepare for the Centenarian Decathlon
- Chapter 13: The Gospel of Stability – Relearning How to Move to Prevent Injury
- Chapter 14: Nutrition 3.0 – You Say Potato, I Say “Nutritional Biochemistry”
- Chapter 15: Putting Nutritional Biochemistry into Practice – How to Find the Right Eating Pattern for You
- Chapter 16: The Awakening – How to Learn to Love Sleep, the Best Medicine for Your Brain
- Chapter 17: Work in Progress – The High Price of Ignoring Emotional Health
- Epilogue
Chapter 1: The Long Game – From Fast Death to Slow Death
There comes a point where we need to stop just pulling people out of the river. We need to go upstream and find out why they're falling in.
—Bishop Desmond Tutu
Death comes at two speeds: fast and slow. In contrast to gunshot wounds and stabbings, slow-growing conditions like cancer can progress insidiously, and by the time they're discovered could be too late for even the best surgeons to treat.
A century ago, fast death was the most common cause of death; now it's the Four Horsemen of slow death: heart disease, cancer, neurodegenerative disease, and type 2 diabetes/metabolic dysfunction.
Medicine even now is more effective on fast than slow death – we can fix serious spine and brain injuries, replace damaged organs, and wipe out infections with powerful antibiotics – but our approach to chronic diseases is more reactive than proactive, more about relieving symptoms than preventing them in the first place. We're intervening at the wrong point in time, after the disease has already taken hold. By the time we get to a clinical diagnosis (e.g. when a patient's HbA1c test result reaches 6.5%, signifying type 2 diabetes) we're already very late in the game.
This book is about longevity. But there are two ways of measuring longevity:
- Your lifespan, or how long you live. Science has not yet made major breakthroughs allowing us to live to age 150, and oftentimes our later years are plagued with ever-declining health and suffering.
- Your healthspan, in contrast, measures how long you maintain your physical and mental function, staying free of disability and disease.
Disappearing down the road to physical disability, dementia, or long-term disease isn't any of our ideal futures. We want to delay or prevent chronic conditions so we can live longer without disease, rather than lingering with disease. The best way to prevent that is to start thinking about it and taking action now.
Each of the Four Horsemen is complex, a product of multiple risk factors compounding over time. Many of those individual risk factors are relatively easy to reduce or eliminate. And many of these risk factors are vulnerable to the same tactics and behavioral changes in this book.
Chapter 2: Medicine 3.0 – Rethinking Medicine for the Age of Chronic Disease
The time to repair the roof is when the sun is shining.
John F. Kennedy
Medicine is conservative in nature, rooted in tradition and resistant to change and innovation. The author found this out when he was reprimanded for giving a patient livesaving medicine at the appropriate time mathematically, before its scheduled time (when the next nursing shift was due to arrive).
"First, do no harm" (which Hippocrates didn't say anyway) exemplifies the culture of medicine now, which takes the wrong approach with risk. Sometimes risk is significantly asymmetric – doing some harm to prevent a much larger one (e.g. death) is warranted.
One of the most egregious examples of medicine getting risk wrong is with hormone replacement therapy (HRT) for postmenopausal women. In 2002 a large clinical trial reported a 24% increase in breast cancer risk in a subset of women taking HRT, and the therapy almost instantly became taboo worldwide as dangerous, cancer-causing. But that risk increase was relative – only a 0.1% increase in absolute terms – yet was deemed to outweigh any benefits, such as preventing hot flashes, night sweats, loss of bone density and muscle mass, and even Alzheimer's disease.
Medicine has gone through three phases in history.
Medicine 1.0, exemplified by Hippocrates and lasting for another two thousand years after his death, was based on direct observation and guesswork.
Medicine 2.0 started in the mid-19th century with the germ theory of disease, though it took centuries to take hold – Semmelweis, who theorized that doctors themselves were passing illness by not washing their hands, was ostracized by the medical community and died in an insane asylum.
With Medicine 2.0 came a new way of thinking – the scientific method: observing, forming a hypothesis, then rigorously testing that hypothesis to determine if it's correct. Penicillin's discovery in 1928 paved the way for the eradication of polio and smallpox, containment of HIV/AIDs in the 1990s, curing hepatitis C, and the rapid development of several effective vaccines against COVID-19 not even a year after the pandemic started.
But Medicine 2.0 has proven far less successful against the Four Horsemen. Over the last century, mortality rates for infectious diseases declined precipitously (due to antibiotics and improved sanitation), but relatively little otherwise. Medicine 2.0 comes in too late – risk factors like atherosclerosis can begin many decades before the person has a heart attack or stroke, but modern medicine only intervenes after that cardiac "event".
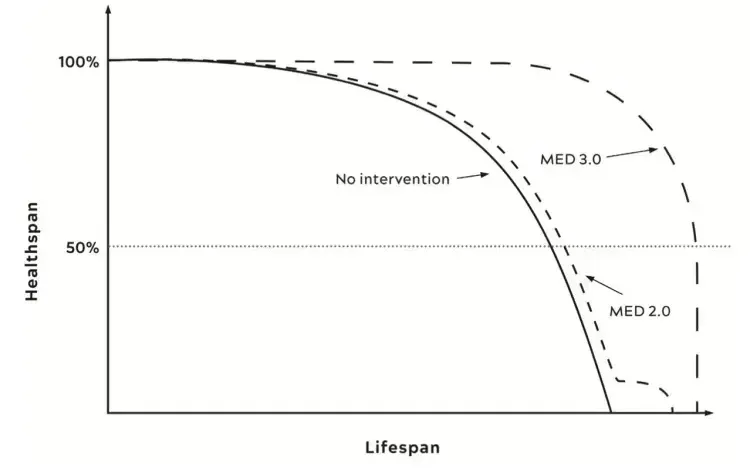
Medicine 3.0 aims to maintain healthspan, the quality of life. It aims to not remove people's tumors and hope for the best, but prevent them in the first place. It treats each patient as a unique individual, instead of relying solely on homogeneous results, the averaged out findings from clinical trials. It determines how each patient is similar or different from "average" and concludes how relevant the trial's results are.
Medicine 3.0 lets us ask how risk and reward balance out on an individual level. How similar or different is our patient from the cohorts studied in the aforementioned HRT clinical trial, and so how relevant are its results?
We have technology now that helps (like continuous glucose monitors/CGMs that can provide visibility into your individual metabolism, as opposed to once-yearly fasting glucose or HbA1c tests) but we're still far from precision medicine, from nanobots injected to treat disease. But Medicine 3.0 isn't about technology; it's a difference in approach.
Longevity and healthspan don't really fit in the business model of our current healthcare system. There are few insurance reimbursement codes for preventative interventions; health insurance companies will pay for (very expensive) insulin after type 2 diabetes diagnosis but not to tell the patient to change the way they eat or monitor their blood glucose levels beforehand.
The Titanic sank because of multiple factors, including ignored telegraph warning messages and the lookout's binoculars locked up with no key. Modern tech like radar and sonar, or GPS and satellite imaging, would have prevented the sinking days in advance. Medicine 3.0 requires looking through a longer lens as well – looking at our 30 or 40 year cardiovascular risk profile, not just the ten-year risk we measure in even the longest clinical trials.
Medicine 3.0 requires the patient to be actively involved – well informed, reasonally medically literate, clear about goals and risk, willing to confront problems rather than ignore them. We need to change ingrained habits, accept new challenges, and venture outside our comfort zone. We're no longer just a passenger on the Titanic; we're the captain.
Chapter 3: Objective, Strategy, Tactics – A Road Map for Reading This Book
Strategy without tactics is the slowest route to victory. Tactics without strategy is the noise before defeat.
Sun Tzu
We need to think about and plan for the later decades of our lives. For many, the last ten years of life is not a happy time – they suffer from one or more Four Horsemen; their cognitive and physical abilities are weakening or gone; they're unable to do the activities they once loved. This Marginal Decade is often a period of diminishment and limitation.
What do we want to do in our later decades? Thinking about this both encourages us to focus on our own endgame (which counters hyperbolic discounting or the preference for immediate gratification) and drives home the importance of healthspan.
"Tactics without strategy is the noise before defeat." Before trying to take a shortcut to the tactics, to exercise, eat, and supplement a specific way, we need to formulate a strategy: an overall approach and mental model tailored to our goals. Understanding the strategy and the science behind it will help us avoid uselessly riding the merry-go-round of fad diets, trendy workouts, and miracle supplements.
Longevity means delaying death from all four Horsemen, and the most common risk factor between them is age – as we age, our immune systems weaken, we develop cardiovascular and respiratory issues, etc. We'll take a closer look at some of the mechanisms behind aging, and into the detailed workings of each of the Horsemen diseases.
The deterioration in healthspan happens in three axes:
- Cognitive decline: our processing speed slows down, our memory begins to fade, and our personality even changes.
- Physical body decline: we lose muscle mass, strength, bone density, stamina, stability, and balance. We could fall and end up in a downward spiral from which we never recover. Many activities require a certain level of muscular and aerobic fitness; even now our V̇O2 max could be barely sufficient, let alone years from now.
- Decline in emotional health: how we deal with distress can have a huge bearing on physical health, happiness, and survival.
Avoiding, slowing, or even reversing all of these is the key way to achieve longevity. Conversely, improving cognitive, physical, and emotional health will reduce our risk of dying more than any medications. Improving healthspan will almost always benefit lifespan as well – increasing muscle strength and improving cardiorespiratory fitness will reduce our risk of dying by much more than taking any cocktail of medications.
Tactics
Medicine 2.0 relies on two types of tactics: procedures (like surgery) and medications. They’re typically applied only when something is already wrong.
Medicine 3.0 tactics fall into five domains: exercise, nutrition, sleep, emotional health, and exogenous molecules (drugs, hormones, or supplements).
- Exercise is the most potent of these five domains, and not only delays actual death but also prevents cognitive and physical decline. Exercise involves four main components: strength, stability, aerobic efficiency, and peak aerobic capacity. All of these must be increased to maximize lifespan and healthspan.
- Nutrition: What you eat matters, but most important is how much you eat – how many calories you take into your body.
- Sleep: If sleep is compromised, a lot goes wrong both in short and long term.
- Emotional health: Why would you live longer if you’re so unhappy?
- Exogenous molecules: The author doesn’t shy away from pharmaceutical drugs because they’re not “natural”. Many drugs, like lipid-lowering medications, are essential items in our longevity tool kit.
From Evidence Based to Evidence Informed
Randomized controlled trials (RCTs) are the gold standard for medical evidence in Medicine 2.0, but are good only for answering questions involving simple interventions (vaccines) or medications (e.g. to lower cholesterol), and over a relatively short period (6 months to 6 years). They won’t tell us much about disease processes that take decades to unfold.
Instead, we take all the data we have – including data that by itself isn’t strong enough to act on – and triangulate a strategy based on that foundation. Our framework shifts from exclusively evidence-based to evidence-informed, risk-adjusted medicine.
We draw from sources of data including:
- Studies of centenarians: people who have lived to 100 or beyond in good health. These are typically observational rather than experimental (so we can’t prove cause and effect) and the sample size is small.
- Animal models like mice. Mice only live 2-3 years so it’s easier to test lifespan-altering tactics, but the downside is discoveries aren’t guaranteed to be replicable in humans.
- Human studies of the Horsemen. How do they begin and progress; what risk factors cause or fuel them; what underlying factors do they share?
- Knowledge about the molecular and cellular changes that occur during the aging process and specific diseases, which help us manipulate them using drugs or behavioral changes.
- Analyses done using Mendelian randomization. If we know specific genetic variations that are associated (but don’t share a common cause) with low vs. high levels of LDL cholesterol, we can study the incidence of cancer and heart disease in populations with and without those variations to derive causality between LDL levels and disease.
None of the above data comes with the certainty that an RCT would provide. But by taking all the information and tools that we have, and thinking in terms of probabilities and risk, we can come up with our own personal health strategy.
Chapter 4: Centenarians – The Older You Get, the Healthier You Have Been
Whiskey’s a good medicine. It keeps your muscles tender.
—Richard Overton, 1906-2018
If you ask centenarians about the secret behind their long lives, they’ll tell you it’s because they drink whiskey, smoke cigars, eat bacon and eggs every day.
What do healthy centenarians actually have in common? Genetics seem to matter a lot – if you’re a sister of a centenarian, you’re 8 times more likely than average to reach that age yourself; if you’re a brother, 17 times as likely. Knowing how your relatives died (and when) helps identify the likely “icebergs” in your path to longevity, plus if you are (luckily) related to any centenarians and could have inherited their lucky genes.
Centenarians generally succumb to the Horsemen just like the rest of us – they just tend to develop those diseases decades later in life, if at all. They’re phase shifted – their entire lifespan and healthspan curves have shifted decades to the right.
Female centenarians outnumber males by at least 4 to 1, but on average male centenarians score higher in cognitive and functional tests. The author attributes this to both selection (males are more susceptible to heart attacks and strokes 1-2 decades before females, so the ones that have them are “weeded out”) as well as males generally having more muscle mass, which is highly correlated to longer lifespan and better function.
Could we reap the same benefits from our behaviors that centenarians get from their genes? Studies have only found a handful of genes that are more prevalent among centenarians compared to the general population. (In general, natural selection doesn’t optimize against genes that confer higher risk later in life, since by that time we’ve already had offspring.)
One such gene is called APOE, named after the protein it codes for, apolipoprotein E. Most people have the e3 variant. Those with the e4 variant have a 2-12x higher likelihood of developing Alzheimer’s and a 81% lower likelihood of reaching extreme old age. The e2 variant, on the other hand, is highly correlated with longevity – those with it are 30% more likely to reach extreme old age. Since we know APOE affects glucose metabolism and cholesterol transport (via lipoproteins), we can pay special attention to issues around those processes – which we will in Chapter 6 and 7 respectively.
FOXO3 is another gene which has variants strongly associated with longevity. It’s a transcription factor, regulating how other genes are expressed (activated or “silenced”), and the genes it activates are responsible for many cellular maintenance-related tasks, along with preventing cells from becoming cancerous. FOXO3 can be activated or suppressed by our behaviors – it’s more activated when we are slightly deprived of nutrients or when we are exercising, giving us another path to investigate.
We can’t change our genes (yet), but we can influence our gene expression via environment and behaviors.
Medicine 2.0 has another flaw in how it treats the Horsemen diseases as separate from one another – the NIH has separate institutions dedicated to cancer, heart disease, etc. But aging is the common risk factor for all of them. Our strategy must incorporate both disease-specific preventions as well as general preventions that target all the Horsemen at once.
Chapter 5: Eat Less, Live Longer? – The Science of Hunger and Health
What we eat and how we metabolize it appear to play an outsized role in longevity.
Soil samples taken from Easter Island in the 1960s led to the discovery and development of the “wonder” drug rapamycin (or sirolimus) a couple of decades later. Now used widely to prevent organ transplant rejection and as a coating for arterial stents, rapamycin acts on an intracellular protein complex called mTOR (“mechanistic target of rapamycin”) which has turned out to be one of the most important mediators of cellular longevity – and one that is found in virtually all forms of life, from yeast to flies to worms to humans.
mTOR helps to balance an organism’s need to grow and reproduce against the availability of nutrients. mTOR is activated when food is plentiful, causing cells to go into growth mode and undergo cell division; when food is scarce, mTOR is suppressed, cells stop dividing, and autophagy occurs – the degradation and recycling of dysfunctional cellular components. Rapamycin acts to inhibit mTOR, triggering the latter process.
In 2009, a study was published in Nature showing that rapamycin improved the remaining life expectancy for “old” mice (~600 days old, equivalent to humans in their sixties) by 28% for males and 38% for females. No other molecule had ever been shown (consistently) to extend lifespan in a mammal, ever – and further studies have confirmed these results in yeast and fruit flies as well.
We’ve known that eating less could promote good health since the 16th century, and studies dating back to the 1930s have experimentally shown that limiting caloric intake can lengthen mammal lifespan. But although caloric restriction does work for some people in improving health, it leaves us more frail and potentially at higher risk for infection so it is far from a panacea. More importantly, caloric restriction research has illuminated critical cellular pathways related to nutrients and longevity – especially pathways triggered when nutrients are scarce which enhance our cells’ stress resistance and metabolic efficiency, all of which are related to mTOR.
One such pathway is an enzyme called AMP-activated protein kinase, or AMPK. It is activated when nutrients are scarce or when we exercise, and triggers the production of new, more efficient mitochondria (which produce energy in the cell) – replacing the older ones damaged by oxidative stress and age. It encourages the liver to produce glucose, releases energy stored in fat cells, and more importantly inhibits the activity of mTOR – triggering the autophagic process of cellular recycling. Through this process, lysosomes in our cells break down old proteins, enzymes, and pathogens, plus destroy protein aggregates (clumps of damaged proteins) which are implicated in Parkinson’s, Alzheimer’s, ALS, and other diseases. Autophagy declines as we get older, and impaired autophagy is thought to be an important driver of numerous aging-related disorders.
Further studies on rapamycin (and its analogs) have demonstrated positive effects beyond autophagy. In 2014, a study was published showing a derivative, everolimus, enhanced the adaptive immune response to the flu vaccine. At moderate to high doses, it acts more of an immune modulator rather than an immunosuppressant.A large clinical trial has begun to evaluate the effects of rapamycin on healthy dogs – and early results suggest it could improve cardiac function and cancer surveillance, reduces systemic inflammation, and have a “rejuvenating function” in some organs.
Although human trials on healthy people may not happen anytime soon for rapamycin (due to side effects and inertia in Medicine 2.0), some people (including the author) have begun taking it off-label for geroprotective (delaying aging) reasons.
Metformin is another drug with potential longevity benefits. Normally taken by diabetics, a large 2014 analysis found that diabetics on metformin have a lower incidence of cancer and live longer than nondiabetics. The FDA has approved a clinical trial (Targeting Aging with Metformin, or TAME) to evaluate metformin’s geroprotective effects, which the author hopes can pave the way for similar studies on rapamycin.
Chapter 6: The Crisis of Abundance – Can Our Ancient Genes Cope with Our Modern Diet?
Avoidable human misery is more often caused not so much by stupidity as by ignorance, particularly our ignorance about ourselves.
—Carl Sagan
Fatty liver disease is normally associated with alcoholics, and manifests as visible nodules of yellow fat and an orangish hue on a liver that is normally a rich purple color. Shockingly, in the last century doctors have seen an epidemic of fatty liver on nonalcoholics, even teenagers – more than one in four people in the world have nonalcoholic steatohepatitis (NASH) or its precursor, nonalcoholic fatty liver disease (NAFLD).
NAFLD and NASH are correlated with obesity and hyperlipidemia (high cholesterol) but early on could have no visible symptoms. Rising levels of the liver enzyme alanine aminotransferase (ALT) in blood tests are the first signs. Although the “acceptable” range for ALT is below 33 IU/L for women and 45 IU/L for men, what is “normal” may not be healthy as the population becomes less healthy. A 2002 study suggests ALT levels below 19 for women and 30 for men instead.
Both NAFLD and NASH are reversible due to our livers’ extraordinary regenerative ability. If you can remove the fat from the liver (e.g. through weight loss) then inflammation will cease and liver function will return to normal. NASH can lead to cirrhosis, however, which is much more difficult to reverse and often requires a liver transplant.
NASH is just one condition in a global epidemic of metabolic disorders, ranging from insulin resistance to type 2 diabetes. These disorders are interrelated, and having any of them (even just NAFLD) puts you at higher risk of both other metabolic dysfunctions and the other three Horsemen diseases – cardiovascular disease, cancer, and Alzheimer’s.
Metabolic syndrome (MetSyn) is the collection of related metabolic problems associated with poor health, and is diagnosed as having three or more of the following:
- High blood pressure (>130/85)
- High triglycerides (>150 mg/dL)
- Low HDL cholesterol (<40 mg/dL in men or <50 mg/dL in women)
- Central adiposity (waist circumference >40 inches in men or >35 inches in women)
- Elevated fasting glucose (>110 mg/dL)
About 90% of the US population has at least one of these, and over 120 million Americans have MetSyn, or at least 3. Note obesity is just one criteria (#4) – between 20-40% of non-obese adults have MetSyn. And this latter group may be in the most serious danger – people with normal weight but metabolic disorders have more than triple the risk of cardiovascular events than metabolically healthy individuals, even obese ones.
Metabolism is how we take in nutrients and break them down for use in the body. In people who are metabolically unhealthy, nutrients and calories end up where they are not needed or even harmful.
Carbohydrates we take in have one of two fates:
- They can end up as glycogen (the easily-accessed storage form of glucose) in skeletal muscle or the liver. Our liver converts glycogen back to glucose and vice versa in a precise manner to enforce a specific balance of glucose in the bloodstream. Our body can store about 1,600 calories of glycogen.
- They can end up as fat, which our body has an almost unlimited capacity to store. Even a relatively lean adult can have 10 kg of fat in their body, representing 90,000 calories of energy.
The decision for where the energy should go relies on hormones, especially insulin. In a sedentary person who isn’t depleting muscle glycogen rapidly, excess energy will largely end up in fat cells. Subcutaneous fat is the safest place to store energy.
When subcutaneous fat energy capacity is exceeded, the body has to find other places to store it, all non-ideal – in the bloodstream as excess triglycerides; in the liver, contributing to NAFLD; in muscle tissue, contributing to insulin resistance in the muscle; even around the heart, pancreas, and around organs in the abdominal cavity (as visceral fat). All lead to an increased risk of cardiovascular disease. Visceral fats secrete inflammatory cytokines in proximity to the most important organs, also increasing the risk of cancer.
People have varying fat storage capacity. Asians tend to have lower capacity than Caucasians. This explains why there are obese people who are metabolically healthy (they’re storing their energy in safe subcutaneous fat) and vice versa. A “thin” person may have a much lower capacity to safely store fat, and therefore less metabolic leeway.
Even small amounts of visceral fat can cause problems. In a 200 pound man, even 4.5 pounds of visceral fat will put him in the top 5% of risk for cardiovascular disease and type 2 diabetes. Doing a DEXA scan annually can illuminate how much visceral fat is there.
Insulin resistance originates in muscle, when droplets of fat accumulate and disrupt insulin-dependent transport mechanisms that bring glucose into the muscle cell. This then progresses to other tissues, and when cells aren’t able to take in more glucose, blood glucose starts to rise – in turn causing the pancreas to overwork, secreting more insulin to try to help. Fat accumulating in the pancreas causes even more pancreatic fatigue and loss of function. Long term hyperinsulinemia (high blood insulin levels) leads to obesity, type 2 diabetes, and all its other consequences. Muscle insulin resistance can be prevented with physical activity.
Another hormone, cortisol, causes a decrease in subcutaneous fat and increase in visceral fat, which is doubly bad. Stress levels and sleep both affect cortisol release, and so managing those are important for metabolism.
Today over 11% of the US adult population has type 2 diabetes, including over 29% of adults over age 65. Another 38% of US adults have prediabetes. This is substantially higher now than before, as our metabolisms aren’t suited to our ultramodern diet – abundant nutrients and calories, similar food availability in the winter, plus an excess of fructose (especially liquid fructose in the form of sugar, high-fructose corn syrup, in juices, yogurt cups, etc) which triggers fat gain more powerfully than any other carbohydrate. Fructose is thought to increase fat gain due to its conversion to uric acid, so uric acid tests are useful to ascertain metabolic health.
Fructose also leads to overeating, as rapid depletion of energy in the cell to metabolize fructose tricks our bodies into thinking it needs more energy. Excess liquid fructose overwhelms our liver’s capability to handle it, quickly ending up as fat. Ironically, many people end up developing NAFLD by drinking too much liquid fructose in the form of “healthy” fruit smoothies.
At the end, excess calories matter the most.
Having any of the markers of metabolic syndrome is a bad sign, and so in Medicine 3.0 we need to start looking for warning signs early:
- Elevated uric acid
- Elevated homocysteine
- Chronic inflammation
- Mildly elevated ALT
- The ratio of triglycerides to HDL cholesterol (less than 2:1 or even better 1:1)
- VLDL levels
The most important is elevated insulin. Insulin resistance is associated with huge increases in cancer risk (12x), Alzheimer’s (5x), and death from cardiovascular diseases (6x). The oral glucose tolerance test (OGTT) tests both glucose and insulin levels after drinking 75 grams of sugar. Normally, blood glucose will spike, followed by a spike in insulin, then both levels will steadily decrease. One in the early stages of insulin resistance would have insulin rise dramatically, then stay elevated or rise even further in the next hour.
Changing how we exercise, what we eat, and how we sleep can completely turn the tables in our favor. But all of these require effort to escape the modern environment which overfeeds, undermoves, and undersleeps us all.
Chapter 7: The Ticker – Confronting—and Preventing—Heart Disease, the Deadliest Killer on the Planet
There is some risk involved in action, there always is. But there is far more risk in failure to act.
—Harry S. Truman
Atherosclerotic cardiovascular disease (ASCVD), which includes heart disease and stroke, is the leading cause of death in the US and the worst killer of the Horsemen. It kills more people than cancer or Alzheimer’s even though it’s more easily prevented than either – we even have a barrage of blood pressure- and cholesterol-lowering medications that are known to reduce the risk of death. We’re losing the war.
A CT scan of the heart, calibrated to detect calcification in the coronary arteries, can be a predictor of future risk of ASCVD.
Cholesterol is essential to life – it’s required in cell membranes, to produce hormones, and to digest food. Blood vessels transport cholesterol throughout the body, wrapped in lipoproteins to dissolve in our blood plasma since it’s not water soluble. HDL (high-density lipoproteins) have more protein proportionally and LDLs (low-density) have more fat. HDLs are encased in apolipoprotein A (apoA) whereas LDLs are encased in apolipoprotein B (apoB).
Cholesterol in food does not impact cholesterol in blood. Don’t be afraid of eating eggs.
Both apoA and apoB can cross the arterial endothelium in both directions, but apoB is more likely to get trapped inside the wall, along with the cholesterol it’s carrying. Stuck LDL (and other apoB-tagged) particles eventually become oxidized, releasing reactive oxygen species which further oxidize the cholesterol and phospholipids they contain and kicking off the atherosclerotic cascade. Oxidized LDL/apoB particles damage the arterial endothelium further, which leads to even greater retention of LDL. The more apoB-tagged particles (LDL, VLDL, etc.) in the bloodstream, the more commonly this cascade happens.
To consume the aggregated LDL, the body sends monocytes (a type of large white blood cell) which transform into macrophages, but consuming too much cholesterol causes them to become foam cells which end up themselves aggregating into a fatty streak which is visible to the naked eye. HDL can reverse this process by “sucking out” the cholesterol back out of the macrophages and returning it to the liver, which is one of the reasons it’s considered “good”. HDL helps to maintain endothelial integrity, lower inflammation, and prevent LDL oxidation as well, but its mechanism of action is less known.
The foam cell membranes eventually break down, leading to a mass of lipids called an atherosclerotic plaque. As the plaque grows, it begins to narrow the lumen (the passage through which blood flows), become unstable, and in later stages calcify to prevent further damage – which is finally what is medically detectable in routine calcium scans. (A more advanced CT angiogram can help find soft plaques prior to calcification.) Unstable plaques that haven’t calcified are the most dangerous, as they can cause the formation of a clot, which can further narrow and block the blood vessel – or break free and cause a heart attack or stroke.
Half of major cardiovascular events occur in people under 65, and as many as a third of 16-20 year olds already have atherosclerotic plaques in their coronary arteries. Anyone over 15 years old is likely to have fatty streaks in their arteries.
LDL is strongly correlated with cardiovascular event risk; HDL function seems to reduce risk but increasing its concentration via drugs doesn’t help. We don’t have any known way to improve HDL function yet.
apoB concentration is far more predictive of cardiovascular disease than LDL. Every standard deviation increase in apoB raises the risk of heart attack by 38%. Get tested for apoB concentration regularly, and get it as low as possible, as early as possible.
Many cases of hereditary “premature” heart disease are caused by another lipoprotein in the apoB family, Lp(a). It is especially deadly as it is more likely than LDL to get stuck in the arterial wall and further causes damage to the aortic valve. Get tested for Lp(a) once, since elevated levels are largely genetic. Lp(a) levels do not respond to behavioral changes, and although PCSK9 inhibitors can help Lp(a) reduce levels by up to 30%, there is no data showing they reduce the chance of cardiovascular events. Beyond that, the only option is to lower the remaining apoB concentration to reduce overall risk.
How to Reduce Cardiovascular Risk
Medicine 2.0 has three blind spots in dealing with atherosclerotic disease:
- Overly simplistic view of lipids that fails to understand how total lipoprotein burden (apoB) truly affects risk (i.e. how much do you need to lower it to achieve meaningful risk reduction)
- Lack of knowledge about other bad actors like Lp(a)
- Failure to fully understand the long term development and prevention of the disease
Test for your apoB and Lp(a) levels. Lower them as much as possible. Keeping LDL-C concentrations around 10-20 mg/dL would probably eliminate the chance of atherosclerosis.
Pay attention to risk markers related to metabolic health – insulin, visceral fat, and homocysteine.
Very low HDL-C is associated with higher risk, but no causal relationship has been proven.
Smoking and high blood pressure damage the endothelium directly, so stop smoking and control your blood pressure.
If triglyceride levels are high, lower them. Eat more monounsaturated fats(up to 60% of overall intake), like extra virgin olive oil, macadamia nuts, and avocados.
Lowering apoB to the levels we want (the levels we have as children) often can’t be accomplished with diet alone, so the author often pairs that with drugs. Statins, which inhibit cholesterol synthesis throughout the body, work for most people. The author starts with rosuvastatin (Crestor). If statins aren’t tolerated, bempedoic acid (Nexletol) can be used – it inhibits cholesterol synthesis only in the liver. Ezetimibe (Zetia) blocks absorption of cholesterol in the GI tract, so it pairs well with statins. PCSK9 inhibitors improves the liver’s ability to clear apoB, and in combination with statins is especially potent. Fibrates help to reduce triglyceride levels when nutritional changes are insufficient. Ethyl eicosapentaenoic acid (Vascepa) could also help reduce LDL in patients with elevated triglycerides.
There is always vascular damage, regardless of how healthy the person seems or how clean their arteries look on scans. Looking at a 30 year time frame, for every 7 people who are put on statins early, 1 life would be saved.
Chapter 8: The Runaway Cell – New Ways to Address the Killer that is Cancer
You may have to fight a battle more than once to win it.
— Margaret Thatcher
Over $100 billion has been spent on cancer research via the National Cancer Institute, but it continues to be the second leading cause of death, and kills Americans at almost the same rate it did 50 years ago.
Once cancer is established, we lack highly effective treatments for it. Surgery and radiation therapy work for local, solid-tumor cancers, but aren’t as effective once the cancer has spread. Chemotherapy slows metastasis but the cancer almost always comes back eventually, and it has significant side effects since we can’t specifically target cancer cells while sparing all normal cells.
It is difficult to detect cancer at an early stage. We typically discover tumors only when they cause other symptoms, by which point they have often already metastasized.
Our three-part strategy is therefore:
- Prevention – avoid getting cancer at all. But we don’t yet fully understand what drives the initiation and progression of cancer, and bad luck seems to play a major role.
- Use newer and smarter treatments targeting cancer’s weaknesses.
- Try to detect cancer as early as possible so our treatments can be deployed more effectively.
Cancer cells don’t stop growing when they are supposed to, and can travel to where they’re not supposed to be in the body. Every instance of cancer starts differently (a different combination of gene mutations, on average over a hundred of them), grows differently, and metastasizes differently.
Cancer Metabolism
Studying cancer metabolism hasn’t been fashionable for long. But even James Watson, one of the discoverers of the structure of DNA, suggested it may be time to look at cancer metabolism – the chemical reactions happening in cancer cells – as well as cancer genetics.
Cancer cells consume huge amounts of glucose, up to 40x the rate of healthy cells. Strangely, even with plenty of oxygen available, cancer cells convert glucose to energy via anaerobic respiration, which is 19x less efficient than normal aerobic respiration. Known as the Warburg effect, there is a hypothesis that this helps cancer cells grow and divide by producing lactate and other chemicals that can be used as building blocks for new cells. (There’s another hypothesis that it protects the tumor from immune cells by reducing the local environment pH via the production of lactic acid.)
Obesity and type 2 diabetes are strongly associated with 13 types of cancers all over the body. Obesity leads to visceral fat accumulation, which releases inflammatory cytokines into the bloodstream and around our organs. Chronic inflammation can make it easier for cells to become cancerous. Insulin resistance (and resulting high insulin levels) help bring substantially more glucose into cancer cells via enzymes called PI3-kinases (PI3K).
This suggests that metabolic therapies, such as diet manipulations, caloric restriction, and improving metabolic health in general may help prevent and slow the growth of cancers in our body.
New Treatments
New drugs inhibiting the PI3K pathway end up raising insulin and glucose levels as more glucose ends up in the bloodstream, counteracting their effect. But combining them with a ketogenic diet (known to minimize insulin) works better – demonstrating both that cancer cell metabolism is a worthwhile drug target, and that the body’s overall metabolic state matters.
Fasting-like diets (providing essential nutrients but very low calorie) improve the effectiveness of chemotherapy on cancer cells, while reducing its impact on normal cells.
The best strategy to target cancer is to target multiple vulnerabilities at the same time, or in sequence.
The Promise of Immunotherapy
Immunotherapy boosts the patient’s own immune system to fight a condition, by killing or neutralizing things not recognized as “self”. Although cancer cells are typically recognized as “self”, there are now therapies that unmask them, making them targets for our T cells.
Currently, immunotherapies only work against a third of cancers, and for only a quarter of patients with those cancers. But when they work, the cancer has a much lower chance of coming back than with chemotherapy.
Early Detection
Too many cancers are detected too late. The ten-year survival rate for patients with metastatic cancer is almost zero, just like it was 50 years ago. The fewer cancerous cells we have, the greater our likelihood of success in treatment.
There are five cancers which have standard, reliable screening methods: lung, breast, prostate, colorectal, and cervical. Although all screening methods have imperfect sensitivity (true positive rate) and specificity (true negative rate), and a large number of false positives, doing screening early enough and using the results effectively can reduce our cancer risk.
It’s far better to screen early than risk doing it too late. The author’s clinic encourages even average-risk individuals to get a colonoscopy by age 40, and repeat it as often as every 2-3 years depending on the results. They recommend doing pap smears yearly, and get checked for skin cancers and melanomas.
Cancers in internal organs are harder to detect, and MRIs and low-dose CT scans only work if the tumor is visible. There are new blood tests that aim to tell you if you have cancer anywhere, and if so, where it most likely is. It’s still early but combining different types of diagnostic tests will hopefully soon tell us if we need treatment, with the fewest false positives.
Chapter 9: Chasing Memory – Understanding Alzheimer’s Disease and Other Neurodegenerative Diseases
The greatest obstacle to discovery is not ignorance—it is the illusion of knowledge.
—Daniel J. Boorstin
Alzheimer’s is the most difficult and intractable of the Horsemen – we have more limited understanding of how and why it begins, how to slow or prevent it, and there’s no way to treat it once symptoms begin. Other neurodegenerative diseases like Lewy body dementia and Parkinson’s disease also affect millions of Americans.
Our only strategy is to try to prevent these diseases. APOE gene testing helps identify Alzheimer’s, Lewy body dementia, and Parkinson’s risk (having the e4 allele as mentioned in Chapter 4).
Understanding Alzheimer’s
Although the phenomenon of “senile dementia” has been known since ancient times, it wasn’t until the 1960s that the mood changes, depression, memory loss, irritability, and irrationality associated with Alzheimer’s were accepted as a physical disease state.
Alzheimer’s disease is known to manifest in the brain as plaques made from aggregated amyloid-beta peptides (caused by improper cleavage of a normal protein called amyloid precursor protein, or APP), and neuronal tangles caused by neurotoxic tau protein aggregation. But targeting amyloid-beta with drugs hasn’t worked well. Confusingly, recent studies have found patients with amyloid plaques but no symptoms, and patients with Alzheimer’s without amyloid plaques.
Lewy body dementia and Parkinson’s are associated with a neurotoxic protein called alpha-synuclein aggregating into Lewy bodies.
Can Neurodegenerative Disease Be Prevented?
The idea that you can prevent Alzheimer’s has been almost taboo in the medical community – the first clinic focusing on Alzheimer’s prevention didn’t open until 2013, and the first randomized control trial showing nutrition, physical activity, and cognitive training can prevent cognitive decline wasn’t published until 2015.
The beginnings of dementia are subtle – and often it’s not recognized until the person goes beyond occasional lapses and forgetfulness to noticeable memory problems. Over 46 million Americans are thought to have stage I preclinical Alzheimer’s disease, which the disease has started its action on our neurons but major symptoms are still absent.
Detecting the early stages of neurodegenerative diseases involves complex tests on executive function, attention, processing speed, verbal fluency, and many forms of memory. It’s tricky to diagnose because our brains can compensate for damage as numerous neural networks are involved in thoughts or insights – and the more of these networks we’ve built (our cognitive reserve), the more we’re resistant to damage.
Alternatives to Amyloid
Beyond plaques and tangles, Alzheimer’s brains also have problems with cerebral blood flow (perfusion). The brain is only 2% of our body weight but uses 20% of our energy, and when blood flow is restricted it develops symptoms of vascular dementia similar to those of Alzheimer’s. Starving neurons of energy starts a cascade of inflammation, oxidative stress, mitochondrial dysfunction, and eventually neurodegeneration.
Another theory is Alzheimer’s stems from reduced glucose metabolism in the brain. Having type 2 diabetes increases Alzheimer’s risk by as much as 3x. Although the brain doesn’t entirely rely on insulin to move glucose, insulin receptors are highly concentrated in the hippocampus, the memory center of the brain. Spraying insulin into people’s noses seems to improve cognitive performance and memory, even in people who have Alzheimer’s.
The Role of APOE e4
APOE codes for a protein (apolipoprotein E) involved in cholesterol transport and glucose metabolism, especially in the brain. The e4 allele has defects in both functions. (Interestingly, the role of e4 in promoting inflammation gives it a converse benefit in fighting infection, so it was the default in all our hominid precursors as it promoted survivability in pre-modern environments.)
e4 carriers are also more likely to develop metabolic syndrome, by disrupting the brain’s ability to regulate insulin levels and glucose homeostasis. It further compounds the brain damage caused by metabolic dysfunction by blocking insulin receptors in the brain, starving neurons of energy.
Other genes like Klotho protect against e4’s negative effects if present.
People at high risk for dementia should pay special attention to their metabolic health.
The Preventive Plan
The first step is to address any metabolic issues present.
A Mediterranean-style diet (more monounsaturated fats, fewer refined carbohydrates, more fatty fish containing the omega-3 fatty acid DHA) can help. Switching to a ketogenic diet lets the brain also rely on ketones for energy (a “flex-fuel strategy”). The role of alcohol on Alzheimer’s is controversial, but cutting it could potentially help.
The most powerful tool is exercise, which helps maintain glucose homeostasis and improves our vascular health.
Steady endurance exercise improves mitochondrial efficiency and reduces cortisol levels, lowers inflammation and oxidative stress, and produces factors that directly target brain regions responsible for cognition and memory.
Strength training is also important. A study of half a million patients showed that grip strength (a good proxy for overall strength) is inversely correlated to dementia risk.
Sleep is also a powerful tool. Our brains heal themselves and clean up waste when we sleep.
Surprisingly, brushing and flossing can help reduce systemic inflammation and possibly Alzheimer’s. The microbe P. gingivalis (that causes gum disease) has shown up in the brains of patients with Alzheimer’s.
Using dry saunas can help. The author suggests at least 4 sessions per week of at least 20 minutes, at 82° Celsius or hotter, to reduce Alzheimer’s risk by 65% and ASCVD by 50%.
Lowering homocysteine with B vitamins, optimizing omega 3 fatty acids, and higher vitamin D levels have shown some promise.
Hormone replacement therapy for women during the transition from perimenopause to menopause seems promising.
The author gives the following principles:
- What’s good for the heart is good for the brain. Vascular health (low apoB, low inflammation, low oxidative stress) is crucial.
- What’s good for the liver (and pancreas) is good for the brain. Metabolic health is crucial.
- Time is key. Think about prevention as early as possible, and play a very long game.
- Our most powerful tool is exercise.
Chapter 10: Thinking Tactically – Building a Framework of Principles that Work for You
Absorb what is useful, discard what is useless, and add what is specifically your own.
—Bruce Lee
Our environment has changed dramatically over the last century, but our genes have remained the same since we were hunter-gatherers. It’s now potentially toxic in what we eat, how we move (or don’t move), how we sleep (or don’t sleep), and its effect on our emotional health.
In Medicine 3.0, we have 5 tactical domains that we can address:
- Exercise is by far the most potent domain
- Nutritional biochemistry, or diet and nutrition
- Sleep
- Emotional health improvement using various techniques
- Exogenous molecules including drugs, supplements, and hormones
When the author evaluates new patients, he asks:
- Are they overnourished or undernourished? (Are they taking in too many or too few calories?)
- Are they undermuscled or adequately muscled?
- Are they metabolically healthy or not?
There is no blanket solution for every person. Learn about the science, look at our own data and biomarkers, come up with a strategy and tactics individually, then iterate over time. Constantly tinker, experiment, switch things up.
Chapter 11: Exercise – The Most Powerful Longevity Drug
I never won a fight in the ring. I always won in preparation.
—Muhammad Ali
Exercise has the greatest power to determine how we’ll live the rest of our lives. It delays the onset of chronic diseases, reverses physical decline, slows or reverses cognitive decline, and benefits emotional health. Going from zero weekly exercise to 90 minutes per week reduces our risk from dying of all causes by 14%. Regular exercisers live a decade longer than sedentary people.
Cardio or weights? The author doesn’t like how we reduce complex, nuanced, vitally important questions into either-ors. Yes, you should do more cardio. And yes, you should lift more weights.
Cardiorespiratory or aerobic fitness is how efficiently your body can deliver oxygen to your muscles, and how efficiently your muscles can extract that oxygen. It’s measured by VO2max, the maximum rate at which you can utilize oxygen (volume per kg of body weight per minute) – and perhaps the single most powerful marker for longevity.
Someone with below-average VO2max for their age group has 2x the risk of all-cause mortality compared to someone in the top quartile, and someone in the bottom quartile has 4x the risk. There is no upper limit of benefit – extremely high aerobic fitness is associated with the greatest survival.
Endurance exercise like running or cycling also helps generate brain-derived neurotrophic factor (BDNF) which improves hippocampus health, responsible for memory.
Muscle is also powerfully correlated with living longer – not just mass but more importantly strength. A study of subjects ages 50+ found that those with low muscle strength have at least double the risk of death than controls. Active people lose less muscle mass as they age beyond 65, and having more muscle mass reduces the risk of falling, by far the leading cause of accidental deaths in people age 65 and older. The fitter you are, the lower your risk of death.
Focusing intensely on a single sport (like cycling) can help improve one metric (like VO2max). Adopting the philosophy of a decathlete – generalists that train like specialists – is the best way to fight our impending decline.
The Centenarian Decathlon
What are the ten most important physical tasks you want to be able to do for the rest of your life? The author presents his patients with a list of physical tasks that could include the following, asking them what they’d want to continue being able to do in their 80s, 90s, etc:
- Hike 1.5 miles on a hilly trail
- Get up off the floor under your own power
- Pick up a young child from the floor
- Carry two 5-pound bags of groceries for 5 blocks
- Lift a 20-pound suitcase into the overhead compartment of a plane
- Have sex
- Climb 4 flights of stairs in 3 minutes
- Open a jar
Typically people want to be able to do all of them. But being able to pick up a great-grandchild means we’ll have to essentially do a squat while holding a 30-pound dumbbell. If our muscle strength declines 8-17% per decade, it means we’d need to be able to do the same with 55 pounds now. Hiking a hilly trail requires a VO2max of 30 ml/kg/min – which will be impossible if our VO2max is 30 now, and it will only get worse.
We need to be able to do much more now to compensate for the decline in strength and aerobic capacity that we’ll suffer as we age.
Come up with the 10-15 things in your own Centenarian Decathlon, then use that as a guide for how you should be training. Instead of being great at one thing, become pretty good at everything. Lose the assumption that we’ll be weak and incapable in our later years, and instead start training with the purpose of being “kick-ass one-hundred-year-olds”.
Chapter 12: Training 101 – How to Prepare for the Centenarian Decathlon
It is impossible to produce superior performance unless you do something different from the majority.
—Sir John Templeton
To delay the onset of chronic disease, while maintaining healthspan for as long as possible, we need to focus on three dimensions of fitness:
- Aerobic endurance and efficiency (cardio): This comprises (1) long, steady endurance work like jogging, cycling, and swimming, i.e. zone 2; and (2) maximal aerobic efforts, i.e. VO2max.
- Strength: Build strength and muscle mass while avoiding injury.
- Stability: Build the foundation that lets us do the rest without getting injured.
Aerobic Efficiency: Zone 2
Zone 2 is aerobic activity between easy and moderate: going at a speed slow enough that you can maintain a conversation, but fast enough that it’s a little strained.
In zone 2, our mitochondria burn fatty acids instead of glucose for energy. Most of the work is done by type 1 or “slow-twitch” muscle fibers, which are dense in mitochondria. Training in this zone helps build healthy and efficient mitochondria and keep fat accumulation in check, as well as providing a base of endurance for anything else we do in life.
If we go beyond zone 2 in intensity, we start using more type 2 or “fast-twitch” muscle fibers, which are less efficient energy-wise. Lactate is created during energy production (glycolysis), which becomes lactic acid if not cleared, making our muscles “burn”.
How you can know if you are correctly in zone 2:
- If you “feel the burn” you are going too hard.
- Your lactate levels (e.g. using a handheld monitor) should be between 1.7 and 2.0 millimoles.
- If you know your maximum heart rate, zone 2 is between 70% and 85% of that number.
- Use the “talk test” – if you’re at the top of zone 2, you should be able to talk but not quite able to hold a conversation.
Zone 2 depends on your fitness – more efficient mitochondria can burn fat and glucose as well as clear lactate more efficiently, preventing the buildup of lactic acid even with higher energy output. In a study, pro cyclists produced ~300 W of power (4 W/kg of body weight) in zone 2, while sedentary subjects produced 100 W (1 W/kg).
People with obesity or metabolic issues have higher resting lactate levels, signifying that their mitochondria are working too hard (and already burning glucose) even to maintain baseline energy levels.
As we age, we lose both number and quality of mitochondria. Aerobic exercise (in zone 2) stimulates the creation of new mitochondria and the recycling of old, dysfunctional ones.
Exercise also triggers pathways that move glucose into muscle cells without insulin – and so is a great way to manage glucose levels for diabetic patients.
There are many ways to reach zone 2 – a brisk walk, riding a stationary bike, walk or jog around a track, swim some laps. Find an activity that fits into your lifestyle, that you enjoy doing, that you can do at a steady pace to stay in zone 2.
For most people, 3 hours per week of zone 2 training (e.g. four 45-minute sessions) is the minimum required to derive benefits. Track the progress of your training by measuring your average output in watts per kilogram.
Maximum Aerobic Output: VO2 Max
At VO2max, we are using both aerobic and anaerobic pathways to create energy, at our maximum rate of oxygen consumption. It is a good proxy of our physical capability and highly correlated with longevity.
Testing VO2max involves riding an exercise bike or running on a treadmill at high intensity, while wearing a mask that measures oxygen consumption and CO2production.
The lower our VO2max, the less we can do. Since it declines as we age (about 10% per decade), unless we start with a high foundation we will eventually find ourselves unable to perform the activities we desire (figure below). Once our VO2max drops low enough (18 ml/kg/min for men or 15 for women), we won’t be able to live on our own.
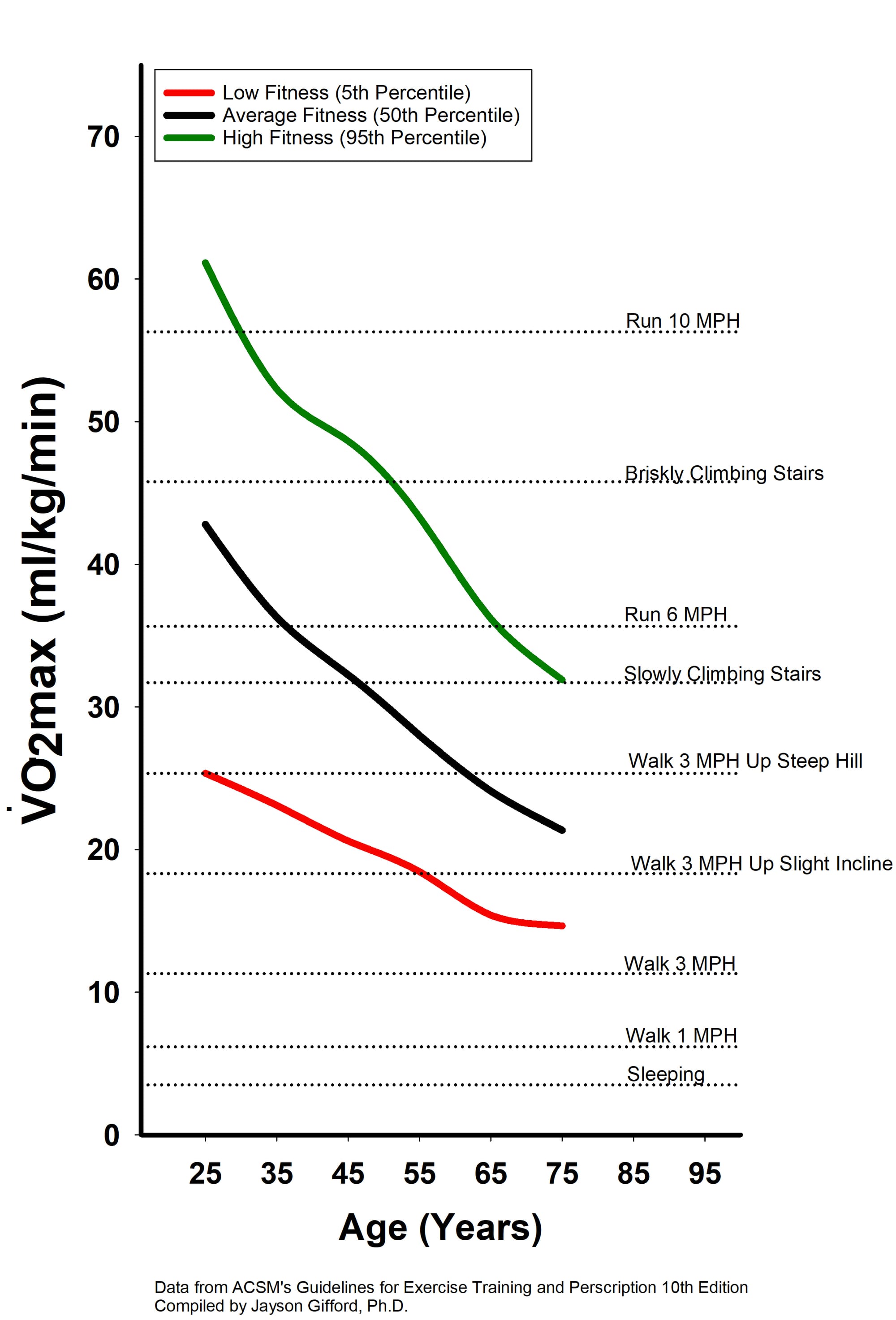
Zone 2 training can benefit VO2max, but the most efficient way to raise it is through long-term, dedicated training. It has a huge payoff – one study found that boosting elderly subjects’ VO2max by 6 ml/kg/min was equivalent to subtracting 12 years from their age.
The author trains by doing 1-2 VO2max workouts per week,doing intervals of 3-8 minutes. Go 4 minutes at the maximum pace you can sustain, then 4 minutes easy (so your heart rate drops below 100). Repeat 4-6 times.
The author has found his ideal VO2max pace is around 33% more power than his zone 2 pace, or 120% of functional threshold power (FTP) for 3 minute intervals or 106% for 8-minute intervals, adjusting for everything in between.
Combining zone 2 and VO2max training is similar to how our hunter-gatherers ancestors lived – 95% slow and steady effort to track and hunt the mammoth, then a huge burst of intensity the last 5% to go in for the kill. We want to be good at going slow for a long time, but also go hard and fast as needed.
Strength
Our muscle mass begins to decline as early as in our thirties, and we lose muscle strength 2-3 times faster than we lose muscle mass. Even worse, due to the atrophy of our type 2 (“fast-twitch”) muscle fibers, we lose power (strength x speed) 2-3 times faster than we lose strength.
Continuous muscle loss as we age terminates in sarcopenia or clinical frailty. It becomes difficult to evenß stand or walk, and one has a huge risk of falling and breaking bones (and the downward spiral that usually leads to).
Another metric that starts to decline in our thirties is bone mineral density (BMD), which can be measured in a DEXA scan. Women who hit menopause without HRT will suffer a faster decline in BMD, since estrogen is essential for bone strength. Slowing this decline is also necessary for protection – up to 1/3 of people over 65 who break their hip are dead within a year.
If a rapid BMD decline is detected in a middle-aged person, the author uses the following strategy:
- Optimize nutrition, focusing on protein and total energy needs
- Strength training with heavy weights, since bones respond to mechanical tension and estrogen mediates that response
- HRT, if indicated
- Drugs to increase BMD, if indicated
The more strength we can build early on, the better off we’ll be in the long term.
In Michael Easter’s book The Comfort Crisis, he claims that since we removed all discomfort from modern life, we’ve lost the fundamental skills that made us human. One such skill is carrying heavy things long distances, and so the author incorporates carries in his strength workouts, using dumbbells, kettlebells, and sandbags. He also goes “rucking” – he fills a rucksack with 50-60 lbs and goes for a walk/hike 3-4 days a week. A good goal is being able to carry 1/4 to 1/3 of your body weight.
The author additionally focuses on training the following, as they are the most relevant to our Centenarian Decathlon, living a fulfilling and active life in our later decades.
- Grip strength: Almost all actions begin with the grip, and it uses all the muscles from your hands to your lats
- Concentric and eccentric loading: Training both when muscles are shortening and lengthening
- Pulling motions: Pull-ups, rows, all angles from overhead to in front
- Hip-hinging movements: Deadlift, squat, step-ups, hip-thrusters, etc. that strength the legs, glutes, lower back
There are a lot of studies linking grip strength to decreased mortality. It’s a good proxy for overall strength, but also helps prevent falls as we get older. Training grip strength can be done using the following exercises:
- Farmer’s carry: Walking for a minute with a heavy weight in your hand, keeping shoulder blades down and back. The author sets a goal for his male patients to be able to carry half their weight in each hand, and female patients 75% of that weight.
- Dead-hanging: Hang from a bar as long as you can. At the age of 40, men should hang for at least 2 minutes, women for 90 seconds.
Training eccentric strength means (sometimes) focusing on the “down” or “negative” phase of lifts, carrying a weighted pack downhill, slowly (3 seconds) stepping down from the box during step-ups and step-downs.
Pulling involves doing rows or using a rowing machine (which the author loves to use for VO2max training too).
Hip-hinging involves exercises that bend at the hips (not spine!) to harness the gluteus maximus and hamstrings.
The author has posted videos with exercises and techniques (and gotchas) on his website.
Chapter 13: The Gospel of Stability – Relearning How to Move to Prevent Injury
The loftier the building, the deeper the foundation must be laid.
—Thomas A. Kempis
Injury and chronic pain are widespread in America. Over 27% of Americans over 45 years old suffer from chronic pain, and 10-12% say pain has limited their activities “most days or every day”. Back pain alone costs $635 billion in medical costs and lost productivity in the US per year.
All the aerobic fitness or strength in the world won’t help you if you get hurt and have to stop exercising for several months (or forever). The author’s first commandment of fitness: First, do thyself no harm.
We must change our mindset – instead of aiming to crush every workout with the most weight or the most reps, we need to focus on doing things right, using safe movement patterns that reduce our risk of injury.
Stability is the key ingredient to avoiding injury – how do we create the most force in the safest manner possible, to use our body’s joints and mechanisms the way they are meant to be used? How do we reduce force dissipation (energy being lost) in our knees, joints, or spine, so they won’t give out at some point?
Many of our posture and stability issues are caused by trying to work around our existing injuries and limitations, then creating new problems. The author starts his patients with stability training before strength training, and he himself does stability training for an hour twice a week, plus 10-15 min per day on the other days.
Dynamic neuromuscular stabilization (DNS, www.rehabps.com) is a program aiming to retrain our bodies and brains to re-learn the perfect movements we learned as kids, like squatting all the way down with knees sharply bent and spines perfectly curved.
Stability training starts with the breath. Breathing both reflects our mental state and affects it, and is important to stability, movement, and strength. Proper breathing affects rib position, neck extension, spine shape, position of feet on the ground.
The author tests all of his patients’ breathing early on as follows:
Lie on your back, with one hand on your belly and the other on your chest, and just breathe normally, without putting any effort or thought into it. Notice which hand is rising and falling—is it the one on your chest, or your belly, or both (or neither)?
Three types of breathing styles each have their own stability strategy:
- “Mr. Stay Puft”: Hyperinflated, upper-chest breather, more susceptible to lower back pain and tightness in calves and hips. Needs to focus on exhaling, getting air out. Work out with weight in front to pull shoulders and hips into a more neutral position.
- “Sad Guy”: Compressed, gravity weighing them down, with head and shoulders jutting forward. Limited neck and upper limb motion. Needs to focus on inhaling with the nose rather than the mouth. Work on cross-body rotation, swinging the arms across the body or doing split-leg work (like a walking lunge with a reach across the body or to the ceiling with each step).
- “Yogini”: Uncontrolled, extreme flexibility but unable to control it. Prone to joint injuries, fidget and twitch, hard to put on lean mass. Do exercises with a well-defined and limited range of motion, like push-ups and exercise machines.
An exercise to build awareness of the breath and strengthen the diaphragm: lie on back with legs up on a bench or chair, then inhale as quietly as possible with the least amount of movement possible. Ideally the entire rib cage (front, sides, back) and the belly all expand at the same time. Then forcefully exhale through almost-closed lips to strength the diaphragm. Pause after each exhale for 2 seconds. Repeat for 5 breaths, 2-3 sets.
Think of the abdomen as a cylinder, surrounded by a wall of muscle, with diaphragm on top and pelvic floor below. When it feels inflated, we’re creating intra-abdominal pressure (IAP) which helps stabilize the spine. When breathing in, try to inflate that cylinder on all sides – expand it around its whole diameter, and pull air all the way down into the pelvic floor. Maintaining IAP is the foundation of stability in everything we do – deadlift, squats, anything.
Our feet are the most fundamental point of contact between our bodies and the world. If our feet roll to the outside (supination), it’s like driving a car with overinflated tires, so we skid and bounce around. If our feet fold inward (pronation), it’s like not having enough air in the tires, so we slosh around, unable to transfer force efficiently to the ground. Any shock our feet don’t absorb ends up transferring to the ankles, hips, knees, and lower back.
Toe yoga involves exercises to improve the dexterity and strength of our toes, plus the ability to control them with our mind. Think of your feet as having four corners, each of which needs to be rooted firmly on the ground at all times: the base of the big toe, base of pinky toe, inside and outside of heel. Then try to lift each toe off the ground separately, or lift all ten toes up and put each toe down separately. See videos about toe yoga at www.peterattiamd.com/outlive/videos. Using “toe spacers” helps restore the toes to a more natural, spread position.
The spine has three parts: lumbar (lower back), thoracic (midback), and cervical (neck). By doing extremely slow Cat/Cow yoga sequences (inhaling on Cow, exhaling on Cat), feeling each individual vertebra changing position, we can build control and awareness of our spine.
Our shoulder joints have a huge range of motion compared to our hips, but their complexity makes them more vulnerable. Shoulder control can be trained with this exercise: stand with feet shoulder-width apart, arms at your sides with some resistance (resistance band under feet, or a light dumbbell). Raise your shoulder blades, then squeeze them back and together, then drop them down, then forward to the starting position. Eventually we can move in circles like this rather than squares.
Our hands are how we transmit force to the world. Finger strength and grip strength are necessary to prevent elbow and shoulder injury. During upper body workouts, focus on initiating movement with the hands and leveraging all the fingers. Train grip strength by doing carries.
All the above concepts and exercises are merely basic stability work. In the author’s medical practice, patients aren’t allowed to work out with heavy loads until they work on all these basic principles for at least six months. Slow down first to go fast later.
Film yourself working out, to compare what you think you’re doing with what you’re actually doing with your body.
The Power of Exercise: Barry
Barry was a successful executive about to turn 80 who started from a base of having not enough physical activity his whole life. He benefitted tremendously from stability and strength training. His exercise progression was as follows:
- Introductory exercises – abdominal breathing, Cat/Cow, balance-related movements, toe yoga, one-leg walking and standing drills
- Building basic strength – walking lunges to fortify lower body, training abdominal strength first with building IAP, then progressing gradually into building upper and mid-body strength
- Drills to improve reaction time and balance, like using an agility ladder
- Jumping drills, which help to avoid bad falls during missteps
- Getting up from the ground with one or no arms. Everyone should be able to do this: https://youtu.be/-Qlvb0TxATc
Chapter 14: Nutrition 3.0 – You Say Potato, I Say “Nutritional Biochemistry”
Religion is a culture of faith; science is a culture of doubt.
—Richard Feynman
Why the author doesn’t like talking about diet and nutrition: they’re “...so poorly understood by science, so emotionally loaded, and so muddled by lousy information and lazy thinking that it is impossible to speak about them in nuanced terms at a party, or say, on social media.”
We don’t actually know much about how what we eat affects our health, leading to a world of numerous self-proclaimed experts and zealous tribes of people insisting their diet is superior with a total lack of evidence: low-fat, vegan, carnivore, Paleo, low-carb, Atkins, etc. The idea that there is a perfect diet that works best for every single person is absolutely incorrect.
Nutrition 3.0 is scientifically rigorous, highly personalized, and driven by feedback & data instead of ideology and labels. Figure out what works for your body and goals, and that you can actually stick to.
We start by answering these questions:
- Are you overnourished or undernourished?
- Are you undermuscled or adequately muscled?
- Are you metabolically healthy or not?
There is a high correlation between poor metabolic health and being overnourished and undermuscled. For the majority of people, the goal will be to reduce energy intake while adding lean mass – consume fewer calories while increasing protein intake.
Undernourished people typically aren’t taking in enough protein to sustain muscle mass.
It’s important to differentiate between what we do to maintain good health, versus what we do to correct poor health and disease. Nutritional interventions that do the latter (highly restricted diets to treat obesity, NAFLD, type 2 diabetes) may not be as applicable to metabolically healthy as something more balanced.
Nutrition has only a few basic rules that we know with complete certainty:
- Don’t eat too many calories, or too few
- Consume sufficient protein and essential fats
- Obtain the vitamins and minerals you need
- Avoid pathogens like E. coli and toxins like mercury or lead
What We Sort of Know About Nutritional Biochemistry (and How We Sort of Know It)
Understanding what kinds of studies are worth heeding and what to ignore is an important first step.
Epidemiological studies involve gathering data on the habits of large groups of people, then looking for meaningful correlations with outcomes such as cancer/cardiovascular disease/mortality. They’ve been useful for epidemics, banning smoking, treating drinking water – but less insightful for nutrition as they can’t distinguish between correlation and causation, which combined with bad journalism causes confusion. Drinking diet sodas is correlated with abdominal fat, hyperinsulinemia, and cardiovascular risk – but which way does the causality go? Could it be that obese people are more likely to drink diet soda because they are heavy, not the other way around?
Sir Austin Bradford Hill came up with 9 criteria to evaluate the strength of epidemiological findings. From Wikipedia:
- Strength (effect size): A small association does not mean that there is not a causal effect, though the larger the association, the more likely that it is causal.
- Consistency (reproducibility): Consistent findings observed by different persons in different places with different samples strengthens the likelihood of an effect.
- Specificity: Causation is likely if there is a very specific population at a specific site and disease with no other likely explanation. The more specific an association between a factor and an effect is, the bigger the probability of a causal relationship.
- Temporality: The effect has to occur after the cause (and if there is an expected delay between the cause and expected effect, then the effect must occur after that delay).
- Biological gradient (dose–response relationship): Greater exposure should generally lead to greater incidence of the effect. However, in some cases, the mere presence of the factor can trigger the effect. In other cases, an inverse proportion is observed: greater exposure leads to lower incidence.
- Plausibility: A plausible mechanism between cause and effect is helpful (but Hill noted that knowledge of the mechanism is limited by current knowledge).
- Coherence: Coherence between epidemiological and laboratory findings increases the likelihood of an effect. However, Hill noted that “lack of [laboratory] evidence cannot nullify the epidemiological effect on associations”.
- Experiment: “Occasionally it is possible to appeal to experimental evidence”.
- Analogy: The use of analogies or similarities between the observed association and any other associations.
The most important of these is Experiment.
Nutritional “studies” typically fail on effect size, the power of the association. It was published that eating red meats increases one’s risk of colon cancer by 17% – compared to cigarette smoking, which increases lung cancer risk by 1000-2500%, the effect size is miniscule.
The raw data that these studies are based on are also suspect – typically a “food frequency questionnaire” which asks subjects to recall everything they ate the last year in minute detail, an impossible task.
Then underlying reasons we eat what we eat (genetics, social influences, economic factors, education, metabolic health, marketing, religion, etc.) could have just as much effect on outcomes as the specific biochemical effects of the foods themselves.
Finally, study results could be biased by differences in subjects’ baseline health. Maybe “moderate” drinking doesn’t cause improved health outcomes – the correlation exists because healthier people are able to drink more, and people who don’t drink could already have a health-related reason for doing so.
Clinical trials are more rigorous than epidemiology, but have a tradeoff between sample size, study duration, and control (trust that the subjects are following the prescribed diet). Compliance is the key issue with nutrition research and with diets in general: can you stick to it?
Evaluate any intervention through efficacy versus effectiveness. How well does it work under perfect conditions and adherence (efficacy)? And how well does it work under real-world conditions, in real people (effectiveness)?
One of the best (least bad) clinical trials showed a clear advantage for the Mediterranean diet – nuts and olive oil. One group of subjects was given a weekly “gift” of a liter of olive oil (encouraging them to eat things that one would prepare with olive oil), another group given a quantity of nuts each week and told to eat an ounce per day, and finally a control group told to eat a lower-fat diet without nuts or fish. The group with olive oil had a 31% lower incidence of stroke/heart attack/death than the control group, and the nuts group had 28% reduced risk.
Does this mean a Mediterranean diet is best for everyone, or that EVOO is the healthiest type of fat? Possibly, but not necessarily. Another issue with diet and nutrition studies in general is the degree of variation between individuals – if only average weight loss is looked at, it misses any sub-group with dramatic weight loss (whose personal metabolisms work very well with what’s being tested) amid the rest losing none or gaining weight.
Chapter 15: Putting Nutritional Biochemistry into Practice – How to Find the Right Eating Pattern for You
My doctor told me to stop having intimate dinners for four. Unless there are three other people.
—Orson Welles
The Standard American Diet (SAD) is our default food environment, occupying the middle of the grocery store – corn, flour, sugar, and soybeans turned into boxed, frozen, and bagged products. Its added sugar, refined carbohydrates with low fiber content, processed oils, and calorie-dense foods are devastating to our health. Ample calories are available for the first time in human history, but evolution hasn’t prepared us well for this situation. We become overnourished and low-quality, ultraprocessed ingredients displace other nutrients (like protein) that we need to maintain optimal health.
All “diets” are fundamentally ways to get away from the SAD. They use one or more of these three strategies:
- Caloric restriction (CR): eating less in total, without attention what’s being eaten or when it’s eaten
- Dietary restriction (DR): eating less of something specific (e.g. meat, sugar, fats)
- Time restriction (TR): restricting eating to certain times, up to and including multi-day fasting
If you’re overnourished (2/3 of us are), you’ll need to apply at least one of these methods
- CR has the highest efficacy, but you have to do it perfectly – can’t cheat or snack – or it doesn’t work.
- DR only works if the food is significant enough that eliminating it will create a caloric deficit. You can still overeat on chips even if you go vegan.
- TR is easy in some ways, but can backfire if you overeat in the one meal per day. It’s also easy to end up protein deficient – causing weight loss but mostly due to losing lean mass, while body fat stays the same or even increases.
CR: Calories Matter
If we take in more energy than we require, the surplus ends up in our adipose tissue. If we saturate our “safe” subcutaneous fat, excess fat will spill into our liver, visceral, and muscles.
In human beings, CR diets are also called “calorie counting”. Weight Watchers works this way. It requires you to track what you eat in meticulous detail, and overcome the hunger you’re certain to feel.
Two monkey studies published in 2009 and 2012 seemed to contradict each other: the first showed calorie restricted monkeys lived longer and healthier; the second showed no statistically significant difference. The key difference between the studies was the food that the monkeys ate – the first study had them eating a highly processed food that was 28.5% sugar, whereas the second study’s monkeys ate something more natural (4% sugar). Comparing the studies, we can draw four conclusions:
- Avoiding diabetes and metabolic dysfunction (e.g. by eliminating junk food) is important to longevity.
- There’s a strong link between calories and cancer, with the CR monkeys having a 50% lower incidence of cancer in both studies.
- The quality of your diet may matter as much as the quantity.
- If your diet is high quality already, and you’re metabolically healthy, then slight calorie restriction (don’t eat too much) can be beneficial enough – you don’t need severe caloric restriction.
DR: The Nutritional Biochemistry “Diet”
This is the world of conventional “diets”, where almost all the attention, research funding, and arguing occurs. We have too many choices and too many delicious ways to take calories into our body – we need to put walls around what we can and can’t eat.
We can implement various degrees of restriction depending on our needs. We still need to make sure that we’re not overnourished – eating only steaks and bacon instead of carbs can easily end up in caloric excess.
Restricting protein is probably a bad idea for most people. Replacing carbs with a lot of saturated fats can cause apoB (and cardiovascular disease risk) to spike.
Everyone’s metabolism is different. Similar diets can lead to very different (even opposite) outcomes, so it’s important to experiment to find the best macronutrient mix for ourselves, in a way that we can sustain. Manipulate our four macronutrients – alcohol, carbohydrates, protein, and fat – to find the optimal combination for ourselves.
Alcohol
Alcohol serves no nutritional or health purpose, and is overall a net negative for longevity. It is calorically dense (7 kcal/g, closer to the 9 kcal/g of fat than the 4 kcal/g of protein and carbohydrate), a potent carcinogen, its oxidation delays fat oxidation (hindering us losing fat mass), and consuming alcohol often leads to mindless eating.
If you drink, be mindful about it. Limit alcohol to fewer than 7 servings per week, no more than 2 on any given day.
Carbohydrates
Carbohydrates are our primary energy source. We break them down into glucose, which all cells consume to create energy. Excess glucose is stored in the liver or muscles as glycogen (for near-term use), or in adipose tissue as fat. Insulin regulates this decision, surging when blood glucose spikes.
Elevated blood glucose amplifies the risk of all Horsemen. Repeated blood glucose and insulin spikes can have a negative impact as well.
With a continuous glucose monitor (CGM), we can monitor how our blood sugar levels respond in real time to what we eat, identifying what specific foods cause spikes (>160 mg/dL) and helping us adjust our eating patterns to stabilize our glucose levels. Using a CGM is especially useful in patients with APOE e4, who have big glucose spikes even when relatively young.
Ideally, average glucose stays at or below 100 mg/dL, with a standard deviation of less than 15 mg/dL. This corresponds to a HbA1c of 5.1%. It’s an aggressive goal requiring experimentation and iteration.
Our carbohydrate tolerance is heavily influenced by our activity level and sleep. Psychological stress elevates cortisol which causes the liver to release more glucose into circulation – causing high glucose levels throughout the night.
Other metrics the author measures include weight, body composition (lean to fat mass ratios), and how they change; plus biomarkers like lipids, uric acid, insulin, and liver enzymes.
Various things the author has learned from CGM over the years:
- The more refined the carb, the faster and higher the glucose spike. Carbs higher in fiber blunt the glucose impact. The author eats more than 50g of fiber per day.
- Rice and oatmeal cause a sharp rise in glucose levels. Brown rice is only sightly better than white rice.
- Fructose is often consumed with glucose so fructose-heavy foods will cause blood glucose spikes.
- Timing, duration, and intensity of exercise matter a lot. Aerobic exercise reduces glucose, while high-intensity exercise and weight training will temporarily increase glucose (to feed your muscles).
- Sleeping only 5-6 hours instead of 8 hours leads to a 10-20 mg/dL jump in peak glucose response, and +5-10 mg/dL in overall levels.
- Stress has a surprising impact on blood glucose, especially during sleep or periods long after meals.
- Nonstarchy veggies like spinach or broccoli have no impact on blood sugar.
- Foods high in protein and fat have no effect on blood sugar, but large amounts of lean protein (chicken breast, protein shakes) will increase glucose slightly.
- Stacking the above insights is powerful in both directions. If you’re stressed out, sleeping poorly, and not exercising, be as careful as possible in what you eat.
- Tracking your glucose has a positive impact on your eating behavior – the Hawthorne effect where you modify your behavior upon being watched.
Protein
Protein is not a primary source of energy, but its building blocks (20 kinds of amino acids) form our muscles, enzymes, many important hormones, hair, skin, nails, antibodies in our immune system, and much more. Consuming sufficient (a lot of) protein prevents the loss of muscle mass as we age, and benefits our metabolism and insulin sensitivity.
9 of the 20 amino acids are essential, or they can’t be formed naturally in our bodies – we must consume them.
The US recommended dietary allowance for protein is 0.8 g/kg of body weight – far less than what we need to thrive. The author typically sets 1.6 g/kg/day as the minimum for his patients, with active people eating with normal kidney function eating at least 2.2 g/kg/day.
Someone weighing 180 pounds should eat 180 grams of protein spread out throughout the day. Four servings of protein a day appears to be ideal, with each portion being around 40-45 grams for this 180-pound person, corresponding to a 6 oz serving of chicken, fish, or meat.
Don’t worry about consuming too much protein. It’s almost impossible to consume more than 3.7 g/kg/day (the safe upper limit).
There’s no CGM for protein, so it’s a process of trial and error. Consume enough to maintain muscle mass. DEXA scans or body composition scales can help track lean mass; consume more protein if lean mass is declining.
Plant protein is not as bioavailable as animal protein, since a lot of it is tied up in indigestible fiber. Cooking the plants helps, but the distribution of amino acids is still not as ideal as animal protein – less methionine, lysine, and tryptophan, all of which are essential. Using plant protein therefore requires doing more math to figure out how much is necessary to get enough – 3-4 g/day of leucine and lysine, 1 g/day of methionine.
Fat
Fats are essential in our body. They form most of the brain, are precursors to many hormones, help us feel satiated after eating, and are an efficient fuel for energy. However, they are high in calories (9 kcal/g) and overeating easily leaves one overnourished, raises LDL cholesterol, and raises heart disease risk.
There are three types of fats: saturated fatty acids (SFA), monounsaturated fatty acids (MUFA), and polyunsaturated fatty acids (PUFA). A “saturated” fat has more hydrogen atoms on its carbon chain.
Olive oil and safflower oil are almost entirely MUFA, and palm and coconut oil are almost entirely saturated fat. All foods contain some proportion of all three types.
PUFA can be split further into omega-6 and omega-3 fatty acids, and omega-3 PUFA can be further split into marine (EPA and DHA, from salmon, anchovies, and other oil-rich seafood) and non-marine sources (ALA, from nuts and flaxseed).
Healthy fat consumption involves tweaking the ratios of the fat types. A typical diet contains 30-40% each of MUFA and SFA, and 20-30% PUFA comprising 6-10x more omega-6 than omega-3s.
The author starts his patients off by boosting MUFA to 50-55%, cutting SFA to 15-20%, with PUFA making up the rest. This is typically done by:
- Eating more olive oil, avocados, and nuts
- Cutting back on butter and lard
- Reducing omega-6-rich corn, soybean, and sunflower oils
- Increasing EPA and DHA with marine fat sources or supplements. The target is 8-12% of red blood cells’ membranes composed of EPA and DHA.
Trans fats are artificial fats that contribute to atherosclerosis by raising apoB, and are banned by the FDA now. They show up on ingredient lists as “partially hydrogenated vegetable oils”, i.e. margarine.
The author uses an expanded lipid panel to track how changes in fatty acid consumption affect patients’ cholesterol synthesis and reabsorption, and lipid and inflammatory response. Slight changes in fat intake (especially saturated fats) make a significant difference in lipid/apoB levels in some people but not in others – so experimentation is required.
MUFA should make up most of our dietary fats, but the balance between SFA and PUFA depends on individual factors. Almost everyone needs to take EPA and DHA supplements in capsule or oil form.
TR: The Case for (and Against) Fasting
Fasting is a powerful tool but has potentially serious downsides.
When we’re not eating:
- Insulin drops dramatically since there are no incoming calories.
- The liver is emptied of fat.
- Over 3 days, the body enters “starvation ketosis” where fat stores are consumed for energy. Ultra-high ketone levels reduce feelings of hunger.
- Over a long period, mTOR (the pro-growth and pro-aging pathway) is turned down, and cellular autophagy (recycling) is accelerated. FOXO (cellular repair) genes are activated.
The author believes fasting is useful in some cases (i.e. severe metabolic dysfunction) but isn’t a panacea and needs to be used carefully.
There are three types of time-restricted feeding:
- Short-term eating windows (“intermittent fasting”), when consumption is limited to a specific time frame, like 6-8 hours of the day. For example: skip breakfast, eat a first meal at 11am, finish dinner by 7pm. The author believes the only benefit is the calorie deficit this achieves, which is easier with a narrower window – 18 or 20 hours of fasting, 6 or 4 hours to eat. Downsides include the fact that it’s not long enough to activate mTOR or autophagy, and it’s easy to miss your protein target, especially if you are trying to gain lean mass.
- Alternate-day fasting (ADF), when you eat normally one day and very little or nothing the next. This could help with weight loss, but it may be due to losing more lean mass (muscle) than fat.
- Longer-term fasting which could lead to even more pronounced loss of muscle mass. The author recommends “thinking about whether prolonged fasting periods [are] actually making it harder to maintain muscle mass and physical activity levels, which are known to be very important factors for long-term health”.
For any diet to be sustainable, you must eat enough to maintain lean mass (muscle) and long-term activity patterns.
Fasting should be used carefully and deliberately – mainly for patients for whom nothing else has worked. Cycles of “hypocaloric” fasting – specifically, one week a month of ~700 calories a day, mostly fat – worked for one of the author’s patients who was so overweight that nothing else did.
Conclusion
Bad nutrition can hurt us more than good nutrition can help us.
If you’re overnourished but undermuscled (like most people), eat enough protein, do zone 2 aerobic training (to consume glucose and access energy stored as fat), and get good sleep.
If you have lipoprotein or cardiovascular issues, focus on fats (especially saturated fats) and apoB levels as well. Stop excessive carbohydrate intake (which also increases apoB/triglycerides), especially in the form of fructose-sweetened drinks like sodas and fruit juices.
Come up with a nutrition plan that you can sustain, that improves or maintains all the parameters we care about – blood glucose, insulin, muscle mass, lipid levels, weight.
Chapter 16: The Awakening – How to Learn to Love Sleep, the Best Medicine for Your Brain
Each night, when I go to sleep, I die. And the next morning, when I wake up, I am reborn.
—Mahatma Gandhi
Every animal sleeps – even though it puts them in an extremely vulnerable state to predators. Why? Because it’s absolutely essential.
Even one sleepless night can make you functionally equivalent to legally drunk. Chronic sleep debt (less than 7 hours a night) can increase our susceptibility to many diseases and metabolic dysfunction, and reduce our life expectancy, safety, and productivity. Sleep is also critical to our cognition, memory, and emotional equilibrium.
We need to sleep about 7.5-8.5 hours a night. Those of us who don’t may think we feel fine, but we’ve just gotten used to the constant mental fog and mild exhaustion.
Old-Man Blood
Chronically sleep-deprived Navy SEALs were found to have “old-man blood” – hormone levels and inflammatory markers of men decades older than them. And people who sleep less tend to have older-looking, flabbier skin.
Poor or short sleep increases risk of hypertension by 17%, cardiovascular disease by 16%, coronary heart disease 26%, and obesity 38%. Even a few days of sleep deprivation can cause significant insulin resistance and a 50% reduction in glucose disposal capacity.
The reason could be stress – poor sleep makes us more stressed, which in turn leads to poor sleep. Our “fight or flight” sympathetic nervous system gets activated continuously, releasing cortisol which raises blood pressure and blood glucose. Poor sleep suppresses leptin (the “satiety” hormone) while increasing ghrelin (the “hunger” hormone), making us more likely to eat high-calorie, sugary foods and overeat in general, making the problem worse.
Sleep and Cardiovascular Disease
The sympathetic nervous system constantly being on high alert places significant stress on our vasculature. Sleeping <6 hours a night was associated with a 20% higher risk of heart attack. Sleeping adequately, on the other hand, reduced heart attack risk even in individuals with genetic predispositions for heart disease.
When we are stressed, our resting heart rate (RHR) will be higher and heart rate variability (HRV) will be lower, both bad things.
Sleep and the Brain
We sleep in a well-defined sequence of stages. Each 90-minute sleep cycle consists of the following stages, typically in the order N1-N2-N3-N2-REM:
- We start in N1 light sleep, characterized by theta waves on an EEG, then quickly drop (in minutes) into deeper sleep.
- Sleep spindles and K complexes on an EEG characterize N2 deeper sleep, crucial for synaptic plasticity and memory consolidation (moving short-term memories to long-term storage).
- N3 deepest sleep shows up as delta waves on an EEG, and is the stage where the body repairs and regrows tissues, bone, and muscle, and strengthens the immune system.
- “Rapid eye movement” or REM sleep features beta waves on an EEG (similar to when we are wake), and our bodies are paralyzed while we dream. In this stage, our brain forms new connections, creatively coming up with solutions to problems from the previous day, and consolidates procedural memory (i.e. new ways of moving the body). REM sleep also helps us process emotional memories (so we feel better the next day) and maintain emotional awareness and equilibrium.
Earlier in the night, we have longer N3 and shorter REM sleep in each cycle; as the night progresses, deep sleep duration shortens and REM duration increases. We can sometimes wake briefly in between sleep cycles.
High levels of noradrenaline (the fight-or-flight hormone) prevents our brain from relaxing enough to enter REM.
During deep sleep, our brain also cleans house, flushing out detritus from the intercellular space including amyloid-beta and tau, two neurodegenerative proteins. Not having enough deep sleep leads to amyloid-beta and tau buildup and a higher risk of developing mild cognitive impairment (MCI) and Alzheimer’s. Conversely, successfully treating sleep disturbance could delay MCI onset by as much as 11 years.
Achieving good-quality sleep is essential to long-term brain health.
Assessing Your Sleep
Sleep medications like Ambien typically just induce unconsciousness, without the brain-healing effects of REM or deep sleep. Valium and Xanax are associated with cognitive decline as well.
Tradozone seems to both encourage falling asleep and improves sleep architecture. The author uses it at lower doses, 50-100mg or less. Ashwagandha has had good results as well.
Using a sleep tracker can measure variables like heart rate, heart rate variability (HRV), movement, and breathing rate, and estimate sleep duration and stage with reasonable accuracy.
Tools like the Pittsburgh Sleep Quality Index, Epworth Sleepiness Scale, and the Insomnia Severity Index can be used to assess sleep quality and its impact on our functioning and well-being.
We all differ in “chronotype” – some of us are genetically “morning people” and others not. This could have a basis in evolution by making sure differing members of a tribe have different times they are most alert, making the whole tribe less vulnerable. Teenagers undergo a temporary shift in chronotype, tending to want to go to bed late and sleep in – hence the movement to push school times later.
Obstructive sleep apnea should be evaluated (and ruled out) as it not only affects sleep quality but also poses a cardiovascular and health and dementia risk.
Sleeping Better
Create an environment that is conducive to sleeping well:
- Give yourself enough time to sleep – go to bed at least 8-9 hours before you need to wake up. Fix your wake-up time and don’t deviate from it, even on weekends.
- Make your bedroom as dark as possible, removing all light sources.
- Reduce blue light (LED light) exposure in the evening.
- Start turning off lights in your house a couple hours before you go to bed.
- Use warmer bulbs.
- Phones, tablets, video games bombard us with blue light and activate our minds – so replace them with passive devices like TV, music, and books. Even watching TV before bed does not affect sleep as much as scrolling on our phones.
- Turn off the computer and put away your phone at least 2 hours before bedtime. Don’t bring them to bed with you.
- Keep your bedroom cool – 65°F or 18°C seems to be optimal.
- Taking a warm bath or using a sauna before bed helps our core temperature drop, signaling to our brain it’s time to sleep.
- Cut back on alcohol as it’s metabolized into chemicals that impair sleep. Even drinking heavily two days after learning impairs retention. If you have to drink, drink before 6pm.
- Don’t eat anything less than 3 hours before bedtime – ideally longer. Go to bed slightly hungry.
- Don’t drink coffee to excess or at the wrong time. Coffee’s half life is 6 hours – so drinking a double espresso at 3pm means we still have a full shot of espresso in our system at 9pm. Everyone has a different tolerance to and metabolism for caffeine – 23andme has data related to one caffeine tolerance-related gene. Stop at 1-2 cups only, before noon, if you have low tolerance.
- Cultivate sleep pressure (adenosine buildup as the day goes on; note caffeine blocks adenosine). Taking a nap can be counterproductive as it relieves sleep pressure, so it’s harder to fall back asleep at night.
- Sustained endurance exercise (zone 2) is especially good for sleep pressure. Don’t work out within 2-3 hours of bedtime.
- Strong daylight exposure during the day – e.g. outdoor exercise – additionally helps keep our circadian cycle on track.
- Mentally prepare yourself for sleep. Don’t do anything that creates anxiety (and activates your sympathetic nervous system), like reading work emails or checking the news.
- Meditation also helps turn down the sympathetic nervous system.
- Don’t obsess over your sleep. If you have an alarm clock, turn it away so you can’t see the numbers – clock-watching makes it harder to fall asleep.
- If you’re worrying about poor sleep scores, stop using your sleep tracker for a while.
A good night of sleep depends on a good day of wakefulness – one that includes exercise, outdoor time, sensible eating (no late-night snacking), minimal to no alcohol, proper stress management, and proper boundaries around work and other life stressors.
What if you can’t sleep at all? If you’re lying awake in bed and can’t sleep, stop fighting it – get up, go to another room, do something relaxing, drink noncaffeinated tea, read a boring book until you feel sleepy again. Find something that’s relaxing and enjoyable that serves no function.
If you’re a night-owl chronotype but trying to sleep early, it might not work as well – adjust your bedtime and waking time, if possible.
If you still can’t sleep, try Cognitive Behavioral Therapy for Insomnia (CBT-I).
Chapter 17: Work in Progress – The High Price of Ignoring Emotional Health
Every man is a bridge, spanning the legacy he inherited and the legacy he passes on.
—Terrence Real
“Why would you want to live longer if you’re so unhappy?”
Addiction can take many forms, not merely to drugs or alcohol. It is often related to trauma in one’s past – and can manifest as anger, detachment, obsessiveness, a need to achieve fueled by insecurity.
Emotional health and physical health are closely intertwined. Beyond suicide, many more people let stress and anger erode their health, fall into self-medicating addictions to alcohol and drugs, or engage in other reckless behaviors (known as parasuicide). So many Americans are dying of drug overdoses, liver disease, and suicide that some segments of the American population actually have lower life expectancy now than before.
Living alone, or feeling lonely, comes with a much higher risk of mortality. It’s crucial to feel connected and have healthy relationships with others, and with yourself.
The Trauma Tree framework builds on the idea that undesirable behaviors as adults (like addiction and uncontrolled anger) are adaptations to various types of trauma from childhood. We need to look at the roots to understand the tree completely.
Trauma falls in 5 categories: abuse (physical, sexual, emotional, spiritual); neglect; abandonment; enmeshment (blurring of boundaries between adults and children); and witnessing tragic events. “Little-T” traumas built up over a long enough time can shape a person’s life as much as a major, terrible, “big-T” trauma event.
Trauma is caused by moments of perceived helplessness, or powerlessness.
Trauma and adversity have a blurry boundary but are different – parenting shouldn’t be about making sure children grow up without any adversity at all.
The four branches of the trauma tree are:
- Addiction – to vices like drugs, alcohol, and gambling; also to work, exercise, and perfectionism
- Codependency – excessive physical reliance on another person
- Habituated survival strategies – like a propensity to anger and rage
- Attachment disorders – difficulty forming and maintaining connections or meaningful relationships with others
The branches are often easy to spot; the tricky part is digging down to the roots and beginning to disentangle them. It takes hard work and a really long time.
The Medicine 2.0 approach to mental and emotional health is the DSM-5, the Diagnostic and Statistical Manual of Mental Disorders, which attempts to describe every mental disorder and category in 991 pages and helps to facilitate insurance reimbursement. But finding a complete solution beyond just diagnosing and prescribing (and billing) is much more difficult.
We must address emotional health early on, and it’ll benefit our overall health as well.
In his book I Don’t Want to Talk About It, Terrence Real writes that men are socialized to conceal their depression, channeling it inward or into other emotions like anger, without ever wanting to discuss it. It manifests as a tendency to isolate oneself and a propensity to anger. “90% of male rage is helplessness masquerading as frustration.” Shame is replaced by a feeling of grandiosity, causing life havoc in the long run.
Children don’t respond to a parent’s anger in a logical way. If they see a parent screaming at someone else, children internalize that rage as if it was directed at them. Children can inherit the shame of those around them.
Dealing with one’s past and changing one’s day-to-day behavior takes time. Some tools and changes that can help include:
- Thinking about relationships as a delicate ecosystem. Why poison the environment in which you have to live?
- Being more relational and present. Making sure to spend time with kids, checking in on loved ones’ experience (not just “events”) daily.
- Limiting phone time and work hours to a strict window, refraining from doing work at all some days.
- Reframing: looking at a given situation from someone else’s point of view. This is hard, since our thoughts and feelings are much more immediate and real than anyone else’s. Why is your time, convenience, agenda more important than theirs?
- The Road to Character distinguishes from “résumé virtues” (accomplishments on our CV) and “eulogy virtues” (things our friends and family will say about us when we are gone). Are you accumulating only résumé virtues in your life?
- Fixing your relationship with yourself. “I need to be great in order to feel like I’m not worthless.” Probe the depths of what shaped you, how you adapted to it, and how those adaptations are now serving you.
Daily practice of dialectical behavior therapy (DBT) helped the author with his emotional issues. It aims to break the chain reaction of negative stimulus -> negative emotion -> negative thought -> negative action.
DBT has an overarching theme of mindfulness which helps you work through its four pillars: emotional regulation (getting control over our emotions), distress tolerance (ability to handle emotional stressors), interpersonal effectiveness (how well we make our needs and feelings known to others), and self-management(taking care of ourselves).
The author struggles with emotional regulation and distress tolerance. He sees his distress tolerance as a window, and tries to keep it as wide as possible – with behaviors like exercise, sound sleep, good nutrition, time with family, medications, deep social connections, spending time in nature, recreational activities that don’t emphasize self-judgment. Increasing his distress tolerance helps him regain control over his emotions, which benefits his interpersonal effectiveness.
Mindfulness is detaching oneself from thoughts and emotions – creating a gap between stimulus and response so you’re not simply reacting reflexively to things that happen. Mindfulness also reminds us that when we are suffering, it’s rarely because of some direct cause – it’s because we’re thinking of some painful event in the past or worrying about something bad in the future. The source of the pain is in our own head. As the Buddha said: “your worst enemy cannot harm you as much as your own unguarded thoughts”; and Seneca: “we suffer more often in imagination than in reality”.
What does our inner dialogue sound like? Is it harsh and judgmental? Record voice memos to yourself on the phone after doing anything that could produce self-judgment. Step outside yourself and view the disconnect between your mistakes and how you talk to yourself about those mistakes.
DBT also teaches techniques to recognize, cope with, and not be controlled by emotions, including anger. When the author gets emotionally distressed, he throws ice water on his face, takes a cold shower, or steps into an ice bath – stimulating his vagus nerve and activating his parasympathetic nervous system. Slow, deep breathing helps too – 4 second inhale, 6 second exhale, repeat.
Opposite action overcomes the desire to do one thing (i.e. not a helpful or positive thing) by forcing oneself to do the exact opposite. Don’t wait for your mood to improve to make a behavior change; changing the behavior can change the mood.
Rucking in nature helps the author remain calm and focused. Exposing oneself to geometric patterns in nature can reduce physiological stress.
Weekly therapy helps the author the most – dissecting and discussing the events and issues of the week in minute detail. He also writes in his journal.
Seek pleasurable activities “consistent with your own values”.
As the author progressed in his recovery, he began finding more joy in being than in doing. Paulo Coelho said: “Maybe the journey isn’t so much about becoming anything. Maybe it’s about unbecoming everything that isn’t really you, so you can be who you were meant to be in the first place.”
Epilogue
The Silicon Valley approach to longevity and health is to hack our biology, tinker and experiment with new protocols and gadgets, until we’re perfect little humanoids who live to 120. The author started there from a fear of dying, but realized that longevity is meaningless if your life sucks – and as he recovered his emotional health, he lost that fear of death and instead gained meaning in his journey to outlive.
The author ends with a quote from a friend: “I think people get old when they stop thinking about the future. If you want to find someone’s true age, listen to them. If they talk about the past and they talk about all the things that happened that they did, they’ve gotten old. If they think about their dreams, their aspirations, what they’re still looking forward to – they’re young.”

![[WIP] Wanting: The Power of Mimetic Desire in Everyday Life (Luke Burgis)](/content/images/size/w960/2024/05/51Qy7hYjK0L.jpg)